WHAT IS DIVERTICULITIS
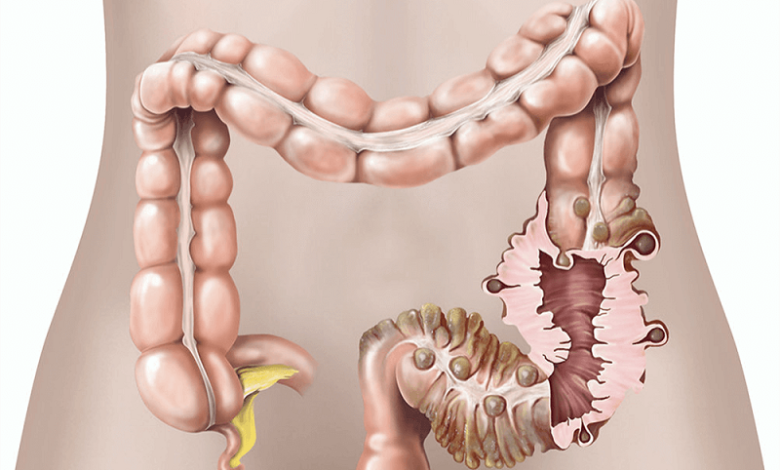
Diverticulitis is an inflammatory process that affects the wall of a diverticulum. Diverticula are sac-like dilations, often described as “glove fingers” that form along the walls of the digestive tract; they are hollow structures that maintain communication with the portion of the gastrointestinal tract from which they originated.
The site in which they form most frequently are the colon and the sigma and can be of two types:
- True diverticula consist of all layers of the intestinal wall and are usually congenital (present from birth),
- While the false diverticula, clearly more frequent, are formed only by mucosa and submucosa and are mostly acquired, generally following a persistent increase in intestinal endo-luminal pressure.
Diverticulitis is a complication of diverticulosis, terms that are often misused as synonyms; in reality, diverticulosis is a condition that in itself only indicates the presence of diverticula, which usually does not manifest itself clinically (ie it does not cause the appearance of symptoms or disorders).
It is not known exactly the cause that triggers the onset of inflammation of the diverticulum, but it is thought that it may originate from an obstruction of the base of the diverticulum by fecal residues or from an ischemic micro-perforation of the diverticulum.
Diverticulitis manifests itself clinically with the following symptoms:
- Clearly definable pain along the lower left side,
- Associated with
- Fever,
- Nausea, vomiting
- And diarrhea .
If not treated promptly and adequately, diverticulitis can give rise to a series of complications, many times even life-threatening, among the main ones are:
- Diverticular abscess,
- Perforation of the diverticulum resulting in generalized peritonitis,
- Intestinal obstruction,
- Intestinal bleeding
- And the formation of fistulas towards adjacent organs.
Diagnosis occurs mainly through the clinic and the use of CT, which also allows distinguishing cases of simple diverticulitis from those of diverticulitis with complications.
Treatment can be conservative in uncomplicated, based cases
- Fast
- Hydration
- And antibiotic therapy,
or it can be surgical in complicated situations or after the second episode of diverticulitis.
CAUSES
It is not known exactly what the underlying cause of diverticulitis is, but one of the most common hypotheses establishes that the cause of diverticulitis is identifiable in the obstruction of the diverticulum by particularly hard and dehydrated fecal material, due to a diet low in fiber. vegetables, rich in red meats and with low water intake, or from a condition of constipation. According to this theory, the occlusion of the diverticulum is followed by a bacterial stasis within the diverticulum which, actively proliferating, involves inflammation of the diverticular mucosa and subsequently a spread of the inflammatory process to the entire wall of the diverticulum.
However, recent studies question this hypothesis, proposing alternatively that the onset of diverticulitis is centered on an ischemic micro-perforation of the diverticulum (lack of oxygen and blood arriving at the diverticulum) due to compression of the nutritional artery at the level of the diverticulum. of the diverticular collar (portion of the diverticulum that connects the lumen of the diverticulum with the lumen of the colon). The alteration of the microcirculation that normally carries oxygen-rich blood to the diverticulum is not fully known, but it is thought to be based on classic cardiovascular risk factors, such as cigarette smoking, obesity, hypercholesterolemia, and absence of physical activity.
The lack of blood and nutrient supply to the diverticulum leads to the formation of necrotic material on which the intestinal bacterial flora can safely proliferate, leading to the onset of diverticular inflammation.
Risk factors
The main risk factors for the development of diverticula and diverticulitis are
- Incorrect and unbalanced diet, especially a diet low in vegetable fiber, excessively rich in red meats and with poor hydration. This results in the formation of harder stools which can obstruct the diverticulum and predispose to its inflammation.
- Constipation , a condition that increases the likelihood that the stool, remaining longer in the colon, becomes excessively dehydrated, becoming particularly dry and hard. This facilitates the obstruction of the diverticula and their secondary inflammation.
- Age : advanced age predisposes the development of diverticula and diverticulitis, due to a progressive reduction in intestinal motility and a generalized weakening of the wall of the entire gastrointestinal system.
- Obesity.
- Cigarette smoke (predisposes to micro-perforations of diverticula on an ischemic basis).
- Lack of exercise and a sedentary lifestyle.
- Family history of diverticulosis and diverticulitis ( genetics ).
- Abuse of nsaids , such as aspirin (acetylsalicylic acid).
Foods containing seeds have in the past been believed to be responsible for the possible triggering of episodes of diverticulitis, but the most recent literature has disproved this hypothesis.
SYMPTOMS
The main signs and symptoms with which an episode of diverticulitis occurs are
- Abdominal pain : this is the main symptom of diverticulitis. It is generally referred to in the left iliac fossa (in the left side below) and tends to be constant, well definable and of variable intensity;
- Fever, usually of a moderate degree. If the fever becomes severe, a complication of diverticulitis, such as peritonitis, must be suspected;
- Alterations of the hive , which can occur both episodes of diarrhea and constipation. Not infrequently there is an alternation of the two manifestations;
- Nausea and vomiting ;
- Abdominal cramps ;
- Abdominal bloating ;
- Meteorism ;
- Blood in the stool , albeit rarely and limited to the most severe cases;
- Urinary disorders , such as difficulty urinating or pain when urinating, are caused by compression of the inflamed diverticulum on the bladder wall or by inflammation of the bladder wall for continuity.
Complications
If not treated properly and promptly, inflammation of the diverticula can give rise to a number of complications, some of which are life-threatening.
Among the main ones we mention:
Abscess : is a collection of purulent material around the diverticulum. It is the most common complication and usually follows microscopic perforations of the diverticulum. It is formed thanks to the immune system that manages to keep the infection in place, in a limited way. It presents with pain localized to the site of the abscess, usually in the lower quadrants. Sometimes the abscess is palpable, although this finding is often masked by the overlying reflex abdominal contracture. Fever is always present, and occasionally nausea and vomiting are also present.
- Perforation: perforation of a diverticulum is a rather rare, but extremely serious and potentially fatal event. It generally arises spontaneously, especially in those cases not treated in an adequate and timely manner, but it is a complication that can potentially affect all cases of diverticulitis. When fecal material leaks into the peritoneal space it causes peritonitis (inflammation of the peritoneum), a serious condition that occurs with
- Sharp pain, usually referred to in the lower abdomen, but with a tendency to rapidly spread throughout the abdomen,
- Abdominal wall contracture,
- Very high fever (greater than 39 ° c),
- Nausea and vomit,
- Tachycardia,
- Intense thirst , due to dehydration .
- Fistulization : abnormal communication between two hollow organs, in the case of diverticulitis between the colon and another organ adjacent to it. Fistulization is the result of the drainage of an abscess into surrounding organs. The most frequent are colo-vesical fistulas (between colon and bladder), while colo-vaginal fistulas (between colon and vagina), colo-cutaneous fistulas (between colon and skin), colo-ileal fistulas (between colon and an ileal loop) and colocolics (between one loop of the colon and the other).
- Intestinal obstruction : condition caused by the inflammatory narrowing of the intestinal segment concerned, or by adhesion phenomena that are formed between the inflamed diverticulum and the contiguous intestinal loops.
- Intestinal haemorrhage : is caused by the diverticular abscess rupture of the perforating branch of the colon’s marginal artery. It is manifested by the presence of dark red blood in the stool.
DIAGNOSIS
The diagnosis of diverticulitis is made through the clinical presentation of the patient and with the execution of the CT scan with a contrast medium; the latter is able to detect
- The presence of diverticulitis, through localized hyperemia of the inflamed diverticulum,
- The presence of complications, such as abscess, perforation, and the presence of abnormal fistulas.
Thanks to the CT scan, it is also possible to classify the severity of diverticulitis, in order to set the most appropriate treatment for each individual case.
TREATMENT AND THERAPY
Diverticulitis therapy differs according to the severity and presence of complications.
In cases of the first attack of diverticulitis and in the absence of complications, therapy is mainly conservative, based on
- Fast,
- Abundant hydration,
- Antibiotic therapy.
On the other hand, subjects who have multiple episodes of diverticulitis or patients with complicated diverticulitis require more invasive interventions, which will differ according to the degree of severity of the diverticulitis and its complications. Less complicated cases are treated with antibiotic therapy and percutaneous drainage of any abscess that has formed, while more serious and complicated cases require intestinal resection surgery of the damaged tract.
Surgery
In rare cases, surgery becomes the only way to prevent or treat the dreaded complications of diverticulitis (fistulas, peritonitis, intestinal obstruction); the objective of the operation is the removal of the affected portion of the intestine (colectomy, performed under general anesthesia ).
It can be practiced in an emergency regime (for example in the case of intestinal perforation) or, when possible, planned and evaluated more calmly; in this second case, the relationship between the risks of surgery and the probability of experiencing complications is usually placed on the scale.
Following the operation, the patient could be given a colostomy, temporary or permanent; it involves the creation of a diversion of the intestine through an opening in the belly that allows the elimination of fecal material through an opening other than the natural one.
DIET
A diverticulitis diet, as defined by the Mayo Clinic, is a temporary measure that involves switching to a liquid-only diet to allow the patient’s digestive system to rest, until bleeding and diarrhea have subsided or resolved.
It is therefore an aggressive approach but limited in time to the acute phase only, which initially involves fasting, excluding clear liquids, the consumption of which is not only allowed but encouraged.
As soon as you start to notice the first improvements, your doctor may advise you to gradually re-enter low-fiber foods, such as:
- Cooked fruit without skin or seeds,
- Cooked vegetables such as green beans, carrots, and potatoes (skinless),
- Eggs, fish, and poultry,
- White bread, rice, pasta, and low-fiber cereals,
- Dairy products if tolerated.
A dietary approach of this type has no particular contraindications, but it should be noted that:
- Fasting must always be agreed upon with the doctor and in any case, limited to a few days to avoid the onset of weakness and other complications (unless it is followed in a hospital setting),
- It must not be chosen independently by the patient before contacting the doctor, who must always evaluate whether a dietary and antibiotic approach is feasible or whether surgery is necessary,
- It should not be confused with the diet for diverticulosis, which instead involves an abundant consumption of fiber in order to prevent the development of diverticulitis.
Once a complete recovery has been achieved, it is recommended to return to insert an abundant content of fiber in the daily diet (at least 30 g per day), taking care to re-insert it very gradually.